
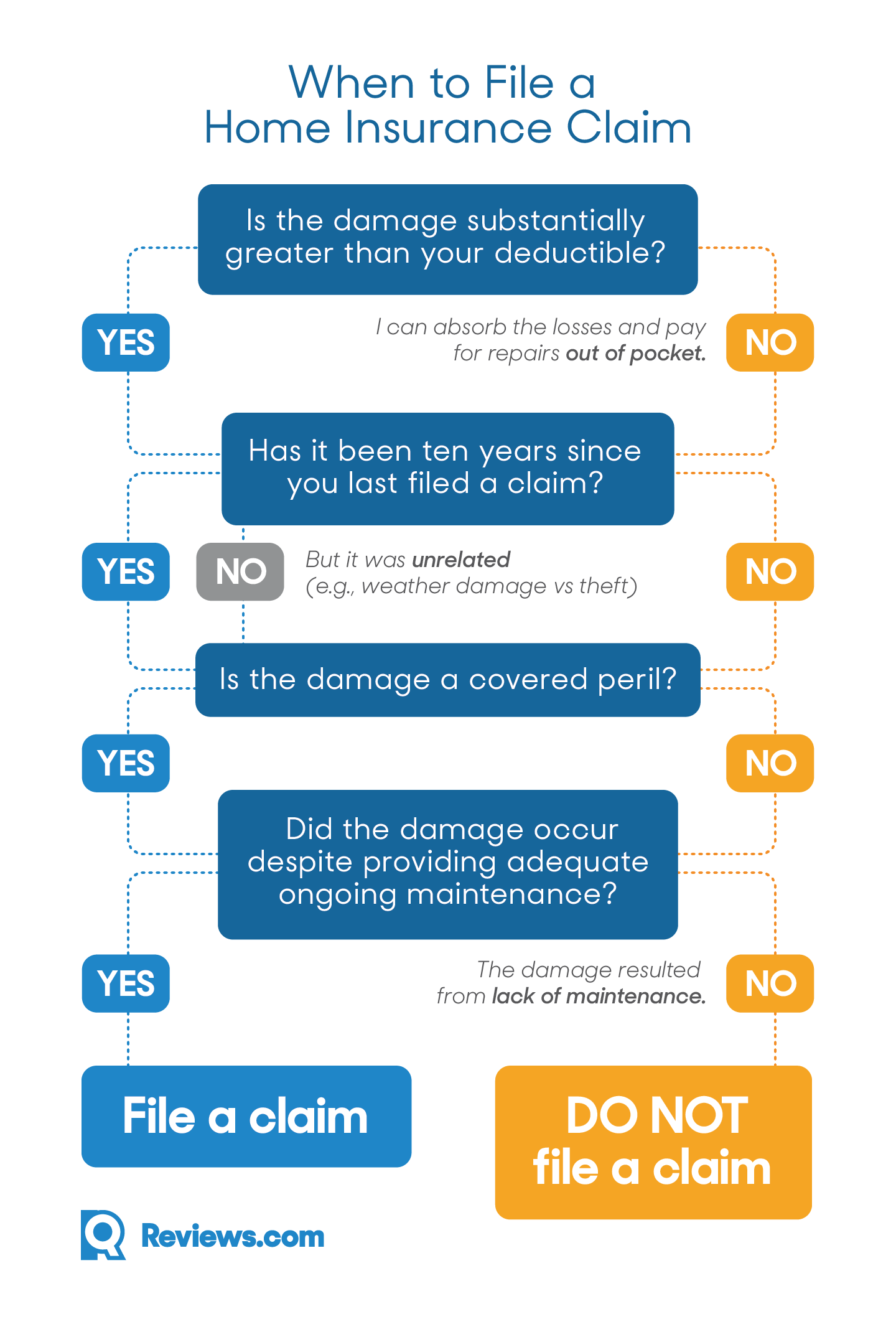
A claims processor will review it for completeness, accuracy, and coverage under your insurance plan. What is the Procedure for Claims Processing? Following your appointment, your doctor will either send a bill to your insurance carrier for any expenses you didn’t pay at the time of the visit, or you will file a claim for the services you got. People also ask, How is a claim processed in healthcare? What is the first step in processing claims successfully? a doctor’s office Payers may seek more information to substantiate claims using a process designed by HIPAA. Payment was made.Īlso, What is the first key to successful claim processing? Review of the handbook The decision on payment. The first processing evaluation is the first of five processes. Secondly, What are the 5 steps to the medical claim process? Repricing ( step 5) Benefits adjudication is the sixth step. What happens when a claim has been submitted? Submission is the first step. Payment has been made.Īlso, it is asked, What are the steps in processing a claim?
#Health insurance claims process flow diagram how to#
When it comes to your insurance policy, your broker is your main point of contact they should be aware of your situation and how to proceed. Step-by-step instructions for your insurance claim Get in touch with your broker. Similarly, What is the first step in processing the claim? Your doctor’s office will send your insurance an itemized statement detailing the treatments you got. Step 1: The path of the health insurance claim starts.
The claims repricing unit reprices the claim and forwards it to the Claims Administrator within three business days for processing.The health care provider submits the claim to the claims repricing unit (The Alliance).The patient visits the health care provider.Within three business days, the claim is sent to the claims administrator for processing and payment, if applicable.įax line for FABOH claims: (608) 210-6677įABOH repricing unit customer service: (877) 837-4245 Medical (except prescription drugs) claims are sent to the FABOH claims repricing unit where the fees on the claim will be re-priced based on the negotiated fee. FABOH members should present their health plan ID card with the FABOH logo when they visit a provider.


 0 kommentar(er)
0 kommentar(er)
